Research
Bionic limb prosthetics – what is it?
Research in the field of bionic limb prostheses represents a cutting-edge research field aimed at revolutionizing the lives of individuals with limb loss. These prostheses, inspired by the principles of bionics, combine advanced technologies and biological principles to create artificial limbs that closely resemble the form and function of natural limbs. A key objective of research in the field of bionic limb prostheses is to provide users with a sense of natural movement and sensation. Advanced technologies such as neural interfaces and myoelectric sensors are employed to establish a direct communication link between the prosthesis and the user’s nervous system. This allows for intuitive control of the prosthesis, enabling users to effortlessly perform complex movements and actions.
Another important aspect of research in the field of bionic limb prostheses is the development of sensory feedback systems. By integrating sensors into the prostheses, researchers aim to provide users with real-time feedback on pressure, temperature, and other sensory information. This sensory feedback allows users to have a more natural and intuitive interaction with their prosthesis, enhancing their overall mobility and quality of life. Furthermore, advancements in materials science and robotics play a crucial role in the development of bionic limb prostheses. Lightweight and durable materials are utilized to create prostheses that are comfortable to wear and can withstand the demands of daily life.
Science Lab
The Science Lab for bionic prosthetics is a specially equipped facility used for research, development, and testing of bionic prosthetics. In this lab, researchers and students can conduct experimental studies to explore and develop prosthetic technologies based on the principles of bionics. It also includes instruments, devices, and technologies required for the development and testing of bionic limbs. These include electromyography systems for capturing muscle activity, sensors for motion and tactile feedback, computer models and simulations for analyzing prosthetic function, and actuators for prosthetic movements. In this laboratory, researchers can conduct experiments to improve the performance of bionic prosthetics, test new materials and design concepts, optimize the interaction between the prosthesis and the user, and explore the integration of sensors and actuators. The goal is to develop advanced prosthetics that allow for more natural movement, fine motor control, and sensory feedback to enhance the quality of life for individuals with limb amputations
Head of the Department Biomedical Engineering Martin Zauner talks about the first Feeling Leg Prosthesis and other research projects
In which areas does the Medical Engineering program at the University of Applied Sciences Upper Austria conduct research?
Zauner: The Medical Engineering program at the University of Applied Sciences Upper Austria is located within the Faculty of Health and Social Sciences. Our main focus in research and teaching is modern medical technology. In addition to prosthetics, research areas include motion analysis and medical simulators, among others. We have specific areas of focus where we further develop research findings and prototypes and make them available accordingly.
What role does research play in application and education?
Zauner: As a university of applied sciences, we are a higher education institution for applied sciences. In our research and teaching, we collaborate with many companies and engage in international research environments through our scientific publications. We serve as a hub for bundling innovations. Naturally, we also strive to implement these innovations in practical applications. Specifically in the field of medical technology, this involves digitization and miniaturization. In the context of prosthetics, we have incorporated these dimensions of innovation to enable not only products for clinical environments but also enhanced everyday usability in the future.
Surgeon Eva Maria Baur talks about Targeted Sensory Reinnervation (TSR) for the first Feeling Leg Prosthesis
What kind of pain can people with amputations experience?
Baur: There are two types of nerve pain that patients may experience. These are neuropathic pain and phantom pain. Neuropathic pain is localized, while phantom pain refers to pain felt in the limb that is no longer present. By redirecting the nerve pathways, it is possible to influence these pains. In this patient’s case, it has been successful. However, it is not possible to say whether this will always be the case from today’s perspective. Pain, especially chronic pain, has its own dynamics. There is, for example, the concept of pain memory, which is not easy to interrupt.
Who benefits from the feeling leg prosthesis?
Baur: I believe the development of the prosthesis is a good thing. It was also important to me that the prosthesis becomes accessible to the general public because there are many more lower limb amputations than upper limb amputations. It is important to me that it doesn’t become a high-tech sports prosthesis, although it would undoubtedly be exciting for a sports medicine specialist. This is about the average consumer being able to move better and more safely. Considering the aging population, the prosthesis is also important. Uneven surfaces or obstacles can soon become a problem for these individuals.
Foot Prosthetics
As the physiologic ankle-foot system is amazingly complex and the foot’s bottom represents the junction of body and floor, foot prostheses play an important role in the fitting process. Unfortunately their significance is frequently underestimated. Prosthetic feet have to be light in weight, but yet of high strength. They should offer a variety of functions such as automatically changing the alignment of the ankle to adapt to different terrains in walking and standing. Furthermore shock absorption in the early stance phase, energy return in the late stance phase and cosmetic are other important design considerations. The alignment of the foot in relation to the socket largely contributes to the overall function.
Knee Prosthetics
A prosthetic knee has to mimic the function of the physiologic knee while providing stability and safety. As the normal gait cycle is divided into two major phases, stance phase and swing phase, prosthetic knees can be classified into two distinct types: those that use mechanical control of the knee joint and those that use microcontroller to control the swing and/or stance phases of gait. While in mechanical knee prostheses the joint’s friction is typically controlled manually, by weight or joint-angle, microprocessor controlled prostheses use sensors (to measure, e.g. force, torque or tilt) that provide a variety of information so that the knee “knows” which gait phase it’s actually in. This allows adapting to different walking speeds, terrain and environmental conditions. Research in this field focuses on control strategies for the wearer’s needs, less weight, high strength, less maintenance and, last but not least, low cost.
Socket
Usually the prosthetic socket comprises a sort of silicon liner, a matching closure system and a load-bearing outer layer. These three components serve as the connection to the knee joint or prosthetic foot. The silicon liner, typically a flexible material, acts as thin protective layer rolled over the residual limb connecting it to the prosthesis. Many manufacturers point out that the sensitive skin is protected in this way because the airtight silicon liner reduces friction and pressure spots. That may be true, but we certainly must not conclude that there are no problems left. A lot of people wearing prostheses complain about sweating and skin irritation due to the airtight silicon liner. Research in this field could focus, e.g. on air permeable textile material reducing skin irritation. Wearer of prostheses would be more than grateful, if an alternative solution was found.
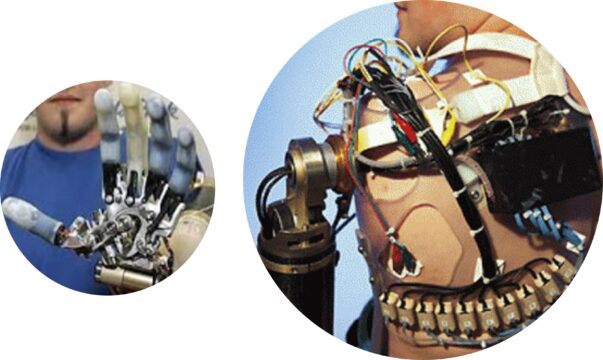
Arm Prosthetics
Upper extremity amputations include finger and partial hand amputations, wrist disarticulation, below elbow, elbow disarticulation, above elbow, and shoulder disarticulation. Three types of socket design determine the suspension: suction, bony lock, and harness, each type having advantages and disadvantages. Hand/Arm prostheses can be passive or active. Often complete passive hand/arm prostheses fulfil only cosmetic purposes not offering any functional benefit. Hooks can be light and efficient; however, they do not look natural. Active prostheses are either body-powered or battery-powered. Typically battery-powered prostheses use myoelectric signals (EMG) for their control. Research in this field focuses on both: to mimic the natural limb as closely as possible and to control it as intuitively as possible.
Prostheses Control Strategy
Myoelectric prostheses are controlled by voluntary muscle contraction. Two battery powered electrode units built into the socket pick up the electromyogram (EMG) created when muscles in the residual limb are contracting; the output of the two electrode units placed on the flexor and extensor muscles deliver control signals SCF(t) and SCE(t) proportional to muscle contraction. These signals turn a single joint’s motor into right and left rotation. A wide-spread method to control more motors consecutively, i.e. more joints with the same signal-pair SCF(t) and SCE(t) is the so-called “co-contraction”: when flexor and extensor muscle are contracting jerky and simultaneously a microcontroller routs the signal-pair SCF(t) and SCE(t) to a second joint’s motor disconnecting the first one. In theory the method can be extended to several joint’s motors, in practice it’s limited by an inacceptable expenditure of time. Research in this field focuses on sophisticated control strategies involving more than two electrode units to control several joints simultaneously.
Targeted Muscle Reinnervation (TMR)
Control based on co-contraction doesn’t allow controlling multiple degrees-of-freedom prostheses simultaneously. By transferring the residual nerves of amputated limbs to muscles out of use more than one signal-pair SCF(t) and SCE(t) can be obtained. Residual nerves delivering natural movement commands control multiple-degrees-of-freedom prostheses in a similar way as they controlled the former natural limbs. Research in this field focuses on sophisticated control strategies like pattern recognition methods using array electrode units to control a multiple degrees-of-freedom prostheses both intuitively and simultaneously.
Targeted Sensory Reinnervation (TSR)
Targeted Sensory Reinnervation (TSR) is an innovative surgical technique developed to enhance sensory perception in individuals with amputations using prosthetics. In TSR, the nerve endings that were previously connected to the amputated limb are redirected to a different target area. The purpose of this redirection is to connect the nerve endings to intact sensory areas. For example, the nerve endings near the amputation site can be connected to sensory nerve endings in the chest or shoulder region. This allows signals captured by the prosthesis to be transmitted to the brain, providing the user with a sense of touch, pressure, or temperature at the location where the prosthesis interacts with the body.TSR can also help reduce or eliminate phantom sensations for the user. By redirecting the nerve endings and establishing a new connection between the nervous system and the prosthesis, the brain receives new sensory information that can diminish phantom sensations.This advanced method requires specialized surgical techniques and careful rehabilitation to optimize the function and integration of sensory reinnervation. However, TSR has the potential to improve the experience of individuals with amputations by providing them with a more natural and enhanced sensory perception with their prosthetics.